Summary
Nava is working with The Centers for Medicare & Medicaid Services (CMS) on their Medicare Payment System Modernization (MPSM) program to create flexible, scalable payment systems that will serve the 65 million people who depend on Medicare. These systems we're working on processed more than $829 billion in Medicare claims in 2021, representing 10 percent of the federal budget and over 3 percent of the national GDP. Though stable, these systems are brittle and difficult to change. Our shared vision is that CMS’s critical systems are able to adapt to evolving Medicare policy and program needs and better serve the people who rely on them.
- Over 1.25 million daily requests representing Medicare claims data processed through our API
- $829 billion in Medicare claims total in 2021
As part of this modernization effort, CMS has been migrating their systems onto the cloud, not only to improve flexibility and scalability but to bolster security and to prepare for the next shock in the system, such as COVID-19. Nava’s Operations and System Reliability Engineering (OSRE) team is dedicated to building and operating the infrastructure for MPSM’s cloud-based services. Our team provides the platform and the infrastructure that CMS developers need to build their applications and serve their needs on the cloud. We also offer guidance and best practices for how to operate their systems, respond to incidents, and evolve in DevOps, Agile, and Security practices. OSRE has also been assisting with strategic design research and infrastructure support as CMS builds a dental claims adjudication process following the expansion of dental coverage under the current administration.
Approach
Alerting teams of tech system outages or incidents
The OSRE team created a system health status page for CMS staff and contractors who are responsible for processing over 1 billion claims a year. The status page centralized and automated the process for alerting CMS staff and contractors when any part of the technology system experiences an outage or other incidents. By using cloud technology to make this information accessible in real-time, the Nava team helped CMS radically improve the speed and transparency of a previously cumbersome process that relied on email communication. The status page seeks to reduce the time it takes to resolve incidents when they occur.
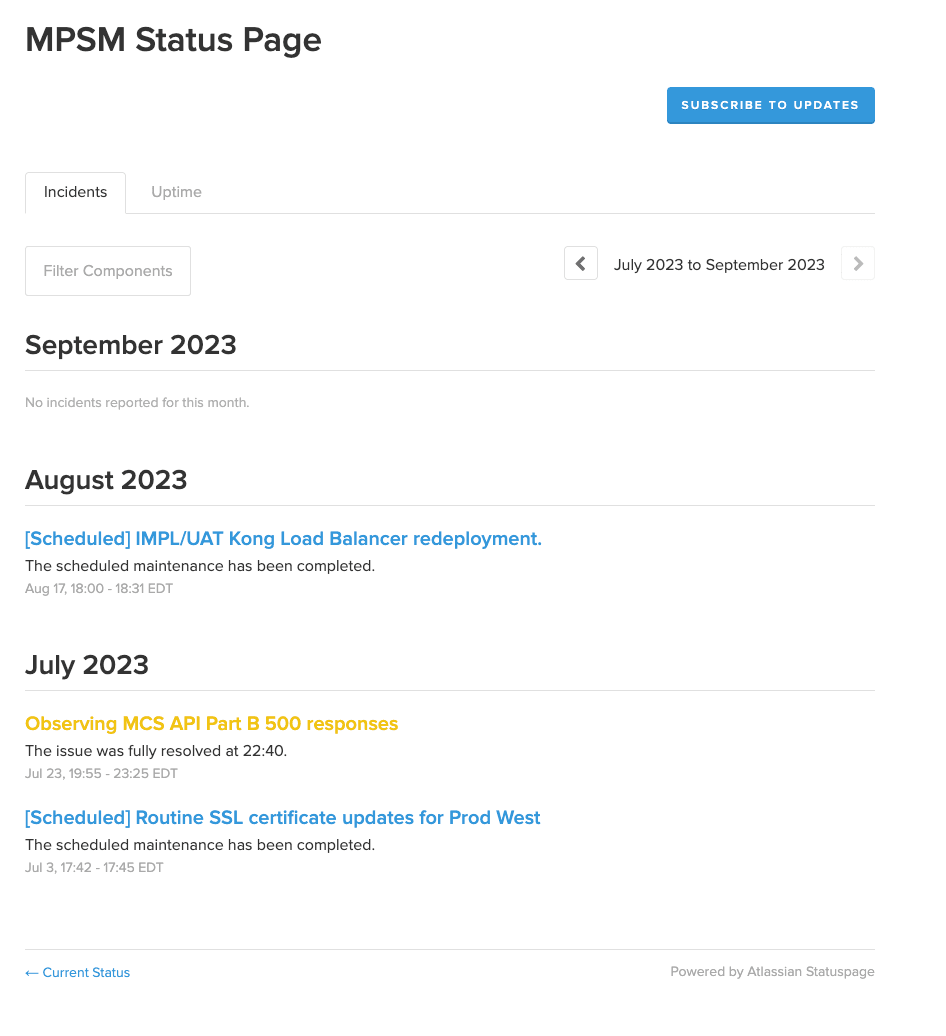
A screenshot of an incident history log on the MPSM status page. It captures scheduled maintenance events as well as one short-lived incident.
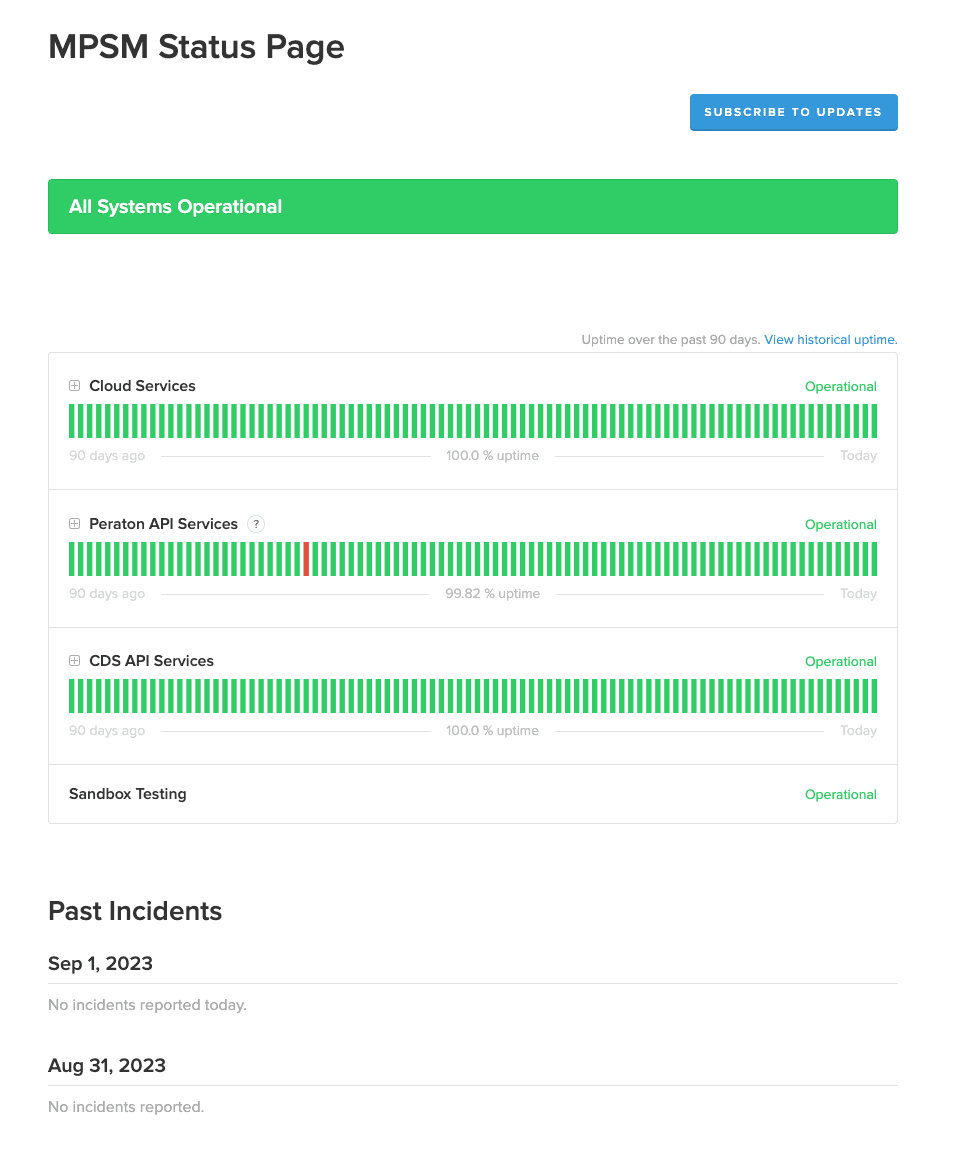
A screenshot of the live health status page where people can see if there are any issues with our services in real time.
Next, the OSRE team helped CMS save costs by moving the incident response tool, where engineers are alerted when system incidents occur, by moving it from PagerDuty to VictorOps. The team integrated this process with Slack to provide yet another layer of automated alerts for some CMS teams. These improvements have continued to streamline the process of notifying CMS staff of potential outages and incidents within the Medicare ecosystem, helping teams get closer to a swift resolution.
Helping to reduce costs through platform and tooling maintenance
CMS’s ongoing modernization project includes empowering new CMS developer teams—called Application Developer Organizations, or ADOs—to onboard their systems and work onto new cloud platforms. When ADOs work on cloud platforms instead of legacy systems, they’re empowered to build, improve, and maintain more flexible, modern, scalable tech infrastructure for Medicare’s payment system. Nava’s team helps support ADOs as they go through the onboarding process, including documentation, security management, and cost optimization.
OSRE also continues to hone cost optimization processes for teams and is working to build tools that can help ADOs identify areas that are ripe for cost savings on their projects. We are working on a process of tagging infrastructure, such as databases, in different tech environments within Medicare’s ecosystem to show how much ADOs are spending on certain infrastructure to highlight potential ways to save costs.
Nava’s team also gathers feedback from ADOs and stakeholders to understand their perception of our customer support platform and platform operations, and to uncover needs, motives, and hopes within MPSM. The goal for this research was to expand understanding of OSRE stakeholders and identify areas for improvement. We’ve used these research findings to help us develop our Developer Experience (DevEx) practice, established to successfully apply human centered and user experience design best practices to OSRE developer-focused processes, tools, teams, and journeys.
Laying groundwork for a new dental claims adjudication process
The Biden administration recently expanded dental coverage under Medicare, extending the definition of medically necessary dental care that is available to Medicare patients. Nava’s teams are working alongside other vendors to support CMS as they build infrastructure and processes that will enable the adjudication of dental claims.
Building on our claims processing experience with other federal and state programs, the Nava team started by mapping out the dental claims adjudication process using a human-centered and service design approach. We supported CMS by building a minimum viable product (MVP) for the cloud-based first adjudication tool dedicated to dental claims for Medicare. As CMS and their vendor partners move into designing and launching this MVP, our team will also support CMS’s infrastructure and other operating needs including platform, networking, and tooling.
We started with research to understand the contexts, relationships, and data contained within a dental claim so that CMS can design a system that truly works for those who use it. We analyzed Medicare taxonomy, dental policy, and interviewed subject matter experts including Medicare Administrative Contractors, Shared System Maintainers, and staff from CMS’s Center for Program Integrity. From there, we moved into simulating a real dental claim—verified by dental experts—to identify rules and processes that are critical to adjudication. The experts were able to uncover open questions in the adjudication process, which helped us understand what's known and unknown in the adjudication of a dental claim.
Based on our research, we identified five business domains for CMS to consider and framed them as human-centered questions, crafting a hypothetical dental scenario and a diagram to help us process the adjudication flow. This framework offers an intuitive way to organize complex information and decipher the potential impacts of decisions being made right now.
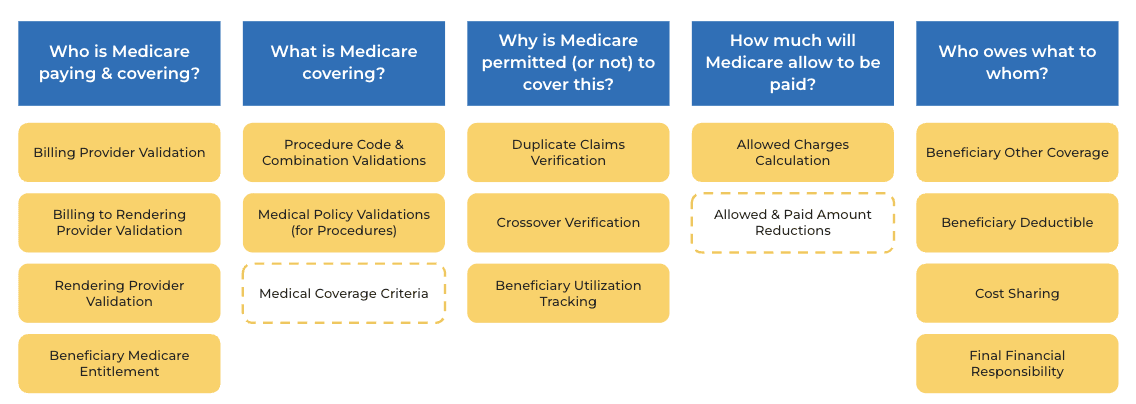
A diagram representing five CMS business domains, framed as human-centered questions.
Focusing on outcomes helps align everyone, regardless of their background or expertise, on the core problems we want our products to solve. This in turn makes the software and operational processes adaptable. When we learn something important about a particular facet of adjudication, we know exactly where to go.
Outcomes
We continue to expand the number of applications supported by the team, providing infrastructure for new ADOs for upwards of seven teams.
In addition, our team built an Application Programming Interface (API) Gateway to connect multiple cloud-based applications to process more than 1.25 million daily requests representing Medicare claims data. This API is part of CMS’s strategy to modernize the Medicare Fee-For-Service system responsible for paying healthcare providers by making pricing information available to the public without compromising the security of claims processing.
Written by

Principal project manager

Strategic communications manager